- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
- Hygeia
- Υπηρεσίες
- Ιατρικά Τμήματα & Υπηρεσίες

Pathology Laboratory

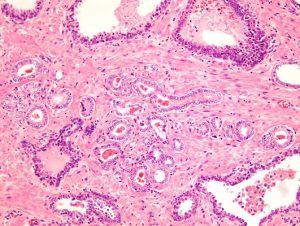
The Pathologoanatomy Laboratory of HYGEIA Hospital is equipped with all modern technological machinery required for the correct preparation and execution of the usual histological examination, but also of the most specialized tests on tissue or cells.Most people know relatively few things about Pathologists and Pathological aka Histological examinations even though these are some of the most critical examinations performed on a patient. The histological examination or biopsy’s result, as it is most commonly known, is the most accurate diagnostic method in medicine and it is particularly important for the patient’s care. For these reasons the histological examinations must be performed in a fully organized and reliable Pathology Laboratory.
HYGEIA Hospital aiming at high quality patient services has a fully organized, staffed and equipped Pathology Laboratory that offers a wide spectrum of examinations.
Meet the HYGEIA Hospital Pathology Department
The HYGEIA Hospital Pathology Laboratory is among the first private pathology laboratories in Greece and is operating since 1974 when HYGEIA Hospital was founded. The laboratory was under the direction of Dr. Despina Georgiadou until 1984 and of Dr. Vassilis Tsakraklidis form 1984 till 2004, two important Greek pathologists. Today Dr. Savvas Papadopoulos is the laboratory’s director and the laboratory is staffed with 12 pathologists, 9 histotechnologists and four secretaries.The laboratory is fully computerized and equipped with the most modern instruments necessary for all procedures (two “enclosed” automated tissue processors, grossing workstation with digital photography and ventilation systems, automated slide stainers, automated coverslipping workstation, two automated IHC/ISH staining instruments) as well as fume hoods and laminar flow cabinets for the protection of the environment and employee’s health.
The Pathology laboratory is actively participating in the weekly scientific meetings of the HYGEIA Hospital Scientific Association and the Hospital’s Tumor Board as well as in research projects mainly in oncology. Several research papers of the laboratory’s physicians have been presented in Greek or international scientific meetings or have been published in Greek or international medical journals.
The Pathology laboratory is collaborating with reliable and internationally recognized pathologists in Europe and the US for particularly difficult or rare cases. Specifically:
- For soft tissue tumors with Prof. Christopher D. M. Fletcher, MD, FRCPath in Brigham’s and Womens’ Hospital, Boston, Massachusetts, USA
- For non neoplastic lung diseases with Prof. Andrew G. Nicholson FRCPath, MD in Royal Brompton Hospital, London, UK
- For general surgical pathology cases with Prof. Juan Rosai in Centro Consulenze Anatomia Patologica Oncologica CDI-Centro Diagnostico Italiano, Milano, Italia
- For central nervous system disorders and tumors with Dr. Pascale Varlet in Laboratoire De Neuropathologie, Centre Hospitalie Saint-Anne, Paris, France.
- Histologic examination of biopsies and surgical specimens of all organs and systems (e.g. stomach, bowel, lungs, breast, prostate, lymph nodes
- Consultation services (histological, histochemical or immunohistochemical examinations)
- Specialized biopsy examination (Fine needle biopsies of thyroid gland, salivary glands, testis, lymph nodes or other palpable tumors)
- Immunohistochemical examination for diagnostic purposes and for the determination of prognostic and predictive factors for all types of cancers
- Molecular morphology and biology examinations (FISH, PCR, RT-PCR, Sequencing) for all types of cancer
- Identification of microorganisms in paraffin embedded tissues with three methods:
1. Histochemistry: bacteria (H Pylori, Mycobacteria), fungi (e.g. cryptococcus), parasites etc
2. Immunohistochemistry: CMV, H. Pylori, HPV etc
3. Molecular testing by PCR: mycobacterium tuberculosis, CMV, HPV, aspergillus, cryptococcus etc
Specialized examinatons for targeted cancer therapyHormonal estrogen and progesteron receptors (ER & PGR): This is an immunohistochemical test performed on tissue removed by biopsy or surgery. With this examination we examine whether the breast tumor is responsive to hormonal therapy.
Her2/Neu oncogene: It is very important for the disease’s course and treatment to know whether this specific gene is expressed by the tumor cells. This test is performed by the method of immunohistochemistry and by thee method of in situ hybridization (FISH, fluorescent hybridization and SISH, silver hybridization). If the gene is present in the tumor there is significant chance that it can be successfully treated with monoclonal antibody based therapy.
Ki-67 (proliferation index): This is an immunohistochemical test and determines the proliferation index of the tumor contributing to the selection of the most appropriate therapy.
PMS2, MSH2, MSH6 and MLH1 proteins: With the study of these proteins we determine whether the patient’s cancer might belong to the microsatellite instability associated tumors and therefore might belong to the inherited colorectal cancers (Hereditary Nonpolyposis Colorectal Cancer, HNPCC) and therefore molecular examination for MSI is subsequently performed.
K-ras, N-ras mutations: These molecular tests are performed in order to determine whether the tumor has mutated K-ras or/and N-ras genes.
BRAF (serine threonine kinase) mutations: This molecular test is performed in order to determine whether the tumor has a mutated BRAF gene or not.
Depending on the results of the above tests the patients may be treated with specific drugs of targeted therapy.
EGFR (epidermal growth factor receptor) mutations: The test is performed in order to determine whether the tumor has mutated EGFR or not. Detection of the expression of this specific receptor or its gene is performed by immunohistochemistry and FISH. Depending on the test’s result the patient receives, or not, treatment with specific drugs of targeted therapy.
ALK (tyrosine kinase): The test to determine whether the tumor expresses this specific gene or protein is performed by immunohistochemistry adn FISH if there is a gene rearrangement. Depending on the test result the patient receives or not specific drugs of targeted therapy.
PDL-1
Immunohistochemical examination for the expression of the PDL-1 cell surface receptor that participates in the deactivation of the immune system (T cells mediated immune response).
Expression of this molecule is important for the immunotherapy of lung and other carcinomas.Immunohistochemical detection of the BRAF protein adn molecular examination for the detection of a mutated BRAF gene (a serine-threonine tyrosine kinase) in all thyroid gland carcinomas and specifically for the papillary thyroid carcinomas for prognostic and therapeutic reason.
Her2/Neu oncogene: It is very important for the disease course and its therapy to know whether this specific gene is expressed by the tumor cells. This test is performed by immunohistochemistry and by FISH (in situ fluorescent hybridization). If the gene is amplified or overexpressed in the tumor there is significant chance that it can be successfully treated with monoclonal antibody based therapy.
This is a group of tumors (sarcomas) of the gastrointestinal tract. They occur at about 55 years of age with a slight predilection for males. The most common site of involvement is the stomach followed by the small and large intestines. These tumors are diagnosed with the help of immunohistochemistry using antibodies against c-kit (CD117) and DOG-1. Detection of specific c-kit mutations (exons 11 and 9) adn PDGFRa mutations is also important for the successfull targeted therapy wiht kinase inhibitors.
Immunohistochemical examination is performed for the classification of these diseases as well as for the selection of appropriate therapeutic options for example administration of anti-CD20 or anti-CD30 monoclonal antibodies in tumors positive for these respectively. In cases of diffuse large B cell lymphoma co-expression of bcl-2 and c-myc is investigated since it is related to the prognosis.
EBER in situ hybridization is the method of choice for the detection of Epstein Barr virus and the results might be decisive for the classification of lymphomas or for the diagnosis of nasopharyngeal carcinoma.
Advisory Services
The experienced laboratory staff are qualified scientists who meet the requirements of ISO 15189 (5.1.2 & 5.1.6). They communicate with all the users of the service offered by the Lab, based on the regulations implemented by the HYGEIA Hospital Clinical Lab Committee. Specifically the Lab:Performs the tests that are selected by each patient’s clinical/attending physician.
- Provides information on the need to perform certain tests that are necessary for the treatment process.
- Offers additional, interpretive notes on the test results.
- Ensures that a test requested by a clinical physician is necessary and useful.
- Gives instructions on patient and sample preparation, as well as the limitations of the requested test.
- Proposes the materials and tests that would lead to useful results for diagnosis and treatment purposes.
- Informs the clinical/attending physician of any deviation from the acceptable limits, which may affect the analysis of the sample.
- Provides additional information on the usefulness and the clinical conclusions arising from the test results.
- Proposes extra tests for the same sample, but using different methodologies, so that the result is documented effectively.
Specimen receipt form outpatients
These tests can be performed either on a paraffin embedded tissue or biopsy/surgical specimen that is placed in a formalin filled container appropriately labeled.
For the performance of all the above tests please consult the following instructions:- For histological consultation by the departments’ doctors of a specimen initially examined in another laboratory the patient should submit the following:
- Histological slides of all sections examined.
- Slides of ancillary techniques (histochemical, immunohistochemical) if they have been performed.
- Paraffin block/s from the most representative area of the lesion in order to perform additional tests if necessary.
- Copy of the histological examination report.
All the above material will be returned to the patient upon completion of the consult. The histological slides of any ancillary technique performed in our lab will be retained.
The material and particularly the histological slides that are fragile must be carefully packaged in specialized containers/mailers supplied by Pathology laboratories. The materials need no refrigaration and can remain at room temperature until receipt.
- For performance of ancillary techniques like detection of oncongenes or their expression products (Her2/neu, EGFR, c-kit, PDGFR, VEGF, MSH, MLH, TS) by FISH, SISH, EBER or immunohistochemistry the patient must submit the following:
- Copy of the histological examination report
- Paraffin block from the lesions most representative area
Upon completion of the examination the paraffin block will be returned to the patient or the patient’s physician.
In case that the materials cannot be delivered in person they can be shipped to the following address:
HYGEIA DIAGNOSTIC & THERAPEUTIC CENTER
PATHOLOGY LABORATORY
ERYTHROU STAVROU 4 & KIFISIAS AVENUE
GR 15123 MAROUSI – ATHENSBefore shipping the specimen, kindly contact the department’s secretariat at 210-6867459 & 210-6867480
Attention:
We would like to inform you that the following speciments are not accepted for examination”
- Fresh tissue for microbiological cultures (e.g. tuberculosis)
- Blood and its products
- Body fluids (pleural effusion, ascites, CSF, sputum)
- Specimen containers without requisition form or accompanying medical report
- Slides or paraffin blocks broken or otherwise compromised or without accompanying histological examination report.
- Specimen containers not appropriately labeled (e.g. patient’s identifiers, specimen type).
All patients have the right to obtain their histological examination report or any other examination performed in our laboratory with the following conditions/means:
- The test should have been financially settled regardless of coverage (insurance or self) and inpatient or outpatient status.
- The most usual way to get results is from the patient’s physician.
- Results from the laboratory are obtained by the patient itself with presentation of his identity card or another individual that provides a notarized (by «ΚΕΠ» or a police department) authorization by the patient and his/hers identity card.
If the patient cannot be physically present or authorize another person due to hospitalization the Hospital where the patient is should provide a written document that certifies the hospitalization and therefore the patient’s inability to present, singed and stamped by the patient’s physician where the name of the person who will receive the results on the patient’s behalf and who needs to present his/hers identity card, is stated. The same procedure is followed for the receipt of biological material (slides-blocks).
NOTE
- The laboratory secretariat is prohibited from communicating the results to patients.
- Delivery of results by fax or email to anybody is stictly prohibited with the exeption of a patient residing overseas when the necessary documents should be submitted to us by email. For more information, kindly contact our Secretariat.
What is the usefulness of a histological examination?
Any disease affecting any part of the body can be diagnosed with a histological examination provided a portion of the lesion could be obtained and forwarded to the Pathology Laboratory for examination. For most diseases, for example cancer, histological examination is the only foolproof diagnostic method.The HYGEIA Hospital pathology laboratory is equipped with the most state-of-the-art instruments available for the appropriate preparation and performance of the usual as well as the most specialized histological examinations in tissues or cells.
What is a histological examination?
The histological examination is the observation of the human tissues under the microscope in order to determine whether there is a disease or not. The tissues can be very small fragments (e.g. those obtained by a gastrenterologist during gastroscopy) up to entire organs resected during surgery (e.g. an entire kidney).Where is a histological examination performed?
Trained specialized physicians called Pathologists perform the histological examination in the Pathology Laboratory of the Hospital.How is a histological examination performed?
The tissues must be appropriately processed before they reach the microscope. Initially the Pathologist places the tissues/organs into liquid fixative in order to dehydrate and preserve them over time. Subsequently the tissues/organs resected are examined, similar to a patient, by touch and visual inspection and records his/her findings, the size, weight, shape, appearance and consistency of the tissues. Primarily though he/she looks for lesions that might be present in the tissues/organs and might indicate the presence of a disease. When a suspicious finding is observed it is recorded and a sample from the lesion is obtained. This procedure is called macroscopic/gross examination and it is the initial and crucial step towards diagnosis.The specimens are subsequently further processed: they are submitted to a sequence of chemical solutions within specialized instruments, are embedded in paraffin, cut into very thin sections and finally stained with specific stains by specialized technologists. It is a time-consuming and demanding process that ensures that the tissues retain all those features necessary for diagnosis. Following this stage the processed tissue/organ specimens arrive again at the Pathologist as very thin sections placed on glass slides in order to be examined with the help of an optical microscope. This is the microscopic examination of tissues. At this point the Pathologist combines all the microscopic findings with the information recorded from the gross examination as well as the clinical information provided by the patient’s physician and reaches a diagnosis.
When a histological examination is performed?
All organs and tissues surgically removed (e.g. stomach, gallbladder, appendix, prostate, uterus) are submitted for histological examination. Especially in tumor cases no treatment is allowed to be administered before histological examination is perforemed and diagnosis is reached.In addition, all visible lesions such as tumor or the skin, mouth, genitals wounds or lesions visivble by X-ray, CT-scan, ultrasound or endoscopically by gastroscopy, colonoscopy, bronchoscope are submitted for histological examination. In such cases the entire lesion or part of it is removed and submitted for histological examination depending on the physician’s decision. Not only the accurate diagnosis is important but also the promptness of examination that allows the timely administration of the appropriate for the patient therapy.
Nowadays the histological examination is performed in minute specimens like those obtained by tru-cut biopsies or fine needle aspirations. With this approach diagnosis is performed with less invasive means-avoidance of surgery and with less cost.
During surgery intraoperative macroscopic/gross and microscopic examination of tissues/organs can be performed if is deemed necessary by the surgeon. This procedure is called “frozen section” and is mostly used in oncological surgeries.
 Contact UsMain building
Contact UsMain building
3rd floorTelephone
+30 210 686 7459
+30 210 686 7480Medical Team
- Director
-
 Papadopoulos Savvas
Papadopoulos Savvas - Associate Directors
-
 Georgiadis Thomas
Georgiadis Thomas -
 Papaioannou Dimitrios
Papaioannou Dimitrios - Assistants
-
 Klimis Thanasis
Klimis Thanasis -
 Margariti Anastasia
Margariti Anastasia -
 Michalopoulou Fani
Michalopoulou Fani -
 Pavlou Kalliopi
Pavlou Kalliopi -
 Stamou Chrysa
Stamou Chrysa
- © 2007-2025 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
























 Photos
Photos 














