- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
- Hygeia
- Υπηρεσίες
- Ιατρικά Τμήματα & Υπηρεσίες
Trigeminal Neuralgia And Chronic Pain
Trigeminal neuralgia is one of the worst pains that humans can suffer.
It is due to abnormal electrical discharges in the cells of the trigeminal nerve and these may be controlled by drugs such as Tegretol and Neurontin. If drugs do not work then surgical techniques are used to damage or decompress the nerve. Such techniques involve the use of cannulae inserted into the skull or require craniotomy. These may be designed to cause permanent nerve damage and carry the risks of open surgery such as infection.
Gamma Knife offers an effective, non-invasive alternative that works even when other methods have failed. A high energy lesion is directed to hit the nerve about 5-8mm from its entry into the brain stem. The dose of radiation can be calculated to stop pain, usually without a significant loss or alteration of sensation. The success depends on the size of the dose and pain is controlled by the first treatment in over 80% of cases.
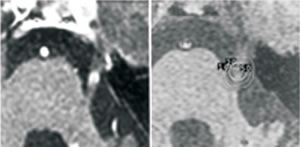 MRI scan of the trigeminal nerve showing the change produced by Gamma Knife treatment (left, arrow) and the dose plan (right) used to achieve it
MRI scan of the trigeminal nerve showing the change produced by Gamma Knife treatment (left, arrow) and the dose plan (right) used to achieve itA Gamma Knife lesion at the root entry zone of the fifth nerve offers a high chance of improvement in drug resistant cases and avoids most of the morbidity of invasive surgical approaches. A multicentre study (1) showed 58% pain free, 36% improved and 6% unchanged. The risk of facial dysaesthesia is 2-4%. If the radiation dose is increased or repeated the cure rate is much higher but so is the risk of mild dysaesthesia. A recent study with a 90Gy dose gave a cure rate of 73% but a 16% incidence of dysaesthesia (2). Giving a second dose to failed cases resulted in an overall cure rate of 98% but all of those given a second dose suffered dysaesthesia (3).
An even more recent study has identified the plexus triangularis, 5-8mm from the brain stem, as a more appropriate target with a cure rate of 83% and dysaesthesia 4% (4).
Post-herpetic trigeminal neuralgia, which does not respond to other surgical treatment (except brain stem DREZ lesions), has been shown to respond to the gamma knife in 44% of cases (5). Since the overall results of Gamma Knife radiosurgery can be better than other techniques it is likely to become progressively more popular.
Chronic pain
In general destructive lesions for the treatment of pain are to be discouraged, but it seems unreasonable to withhold the benefit of medial thalamotomy in cases of cancer pain where all else has failed. 65% of unilateral pain cases are effectively controlled in this way. Hypophysectomy is also useful in bone pain from Ca breast metastases. Both thalamotomy and anterior cingulotomy can chronic pain of non-malignant aetiology but the indications and results are not yet clarified.
REFERENCES
- Kondziolka D, Lunsford LD, Flickinger DC. Stereotactic radiosurgery for trigeminal neuralgia: a multi-institutional study using the gamma unit. J Neurosurg 1996; 84 940-945.
- Nicol B, Regine WF, Courtney C et al. Gamma knife radiosurgery using 90Gyfor trigeminal neuralgia. J Neurosurg 2000; 93(suppl3): 152-154.
- Pollock BE, Foote RL, Stafford SL et al. Results of repeated gamma knife radiosurgery for medically unresponsive trigeminal neuralgia. J Neurosurg 2000; 93 (suppl 3): 162-164.
- Massager N, Lorenzoni J, Devriendt D et al. Gamma knife radiosurgery for idiopathic trigeminal neuralgia: importance of the irradiation dose received by the brainstem. Proceedings EANS (Lisbon) 2003, p127.
- Urgosik D, Vymazal J, Vladyka V, Liscak R. Treatment of post herpetic trigeminal neuralgia with the gamma knife. J Neurosurg 2000; 93 (suppl 3): 165-168.
- © 2007-2025 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.



































