- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
Ankylosing spondylitis
What is ankylosing spondylitis?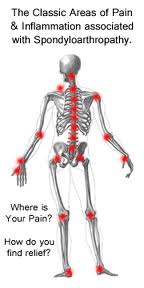
Ankylosing spondylitis (AS) is an inflammatory condition that affects the joints in your spine. Spondylitis simply means inflammation of the spine. It can sometimes affect your other joints and different parts of your body, such as the hips and knees.
As the inflammation settles, calcium is laid down where the ligaments attach to the vertebrae. This makes your back less flexible. Eventually the individual bones of the spine may link up (fuse). This is called ankylosis.
Ankylosing spondylitis varies from person to person – your symptoms might be so mild that you can almost forget you have the condition. it is a fact that sometimes it takes years to diagnose the condition. But when the symptoms are more serious, they could have a big impact on your quality of life.
Ankylosing spondylitis is a type of arthritis called a “spondyloarthritis” (pronounced as spond-ee-lo-arth-ritis), a group of conditions that share many of the same symptoms.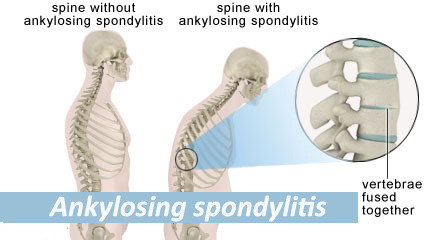
What are the related conditions?
There are a number of conditions related to ankylosing spondylitis which have many similar symptoms. These conditions include:
• undifferentiated spondyloarthritis
• psoriatic arthritis
• spondyloarthritis associated with inflammatory bowel disease (or enteropathic arthritis)
• reactive arthritis
• enthesitis-related juvenile idiopathic arthritis (JIA)What are the symptoms of ankylosing spondylitis?
Typical symptoms of ankylosing spondylitis include:
• lower back or neck pain and stiffness
• pain in your sacroiliac joints (the joints where the base of your spine meets your pelvis). The pain may also be felt in buttocks or the back of your thighs
• tiredness (fatigue)Other possible symptoms include:
• pain and swelling in other joints
• tenderness or discomfort around your heels
• swollen fingers or toes (usually called dactylitis)
• pain or tightness in your chest
• eye inflammation (painful, bloodshot eyes)In the early stages, ankylosing spondylitis is likely to cause:
• stiffness
• pain in your buttocks and sometimes the backs of your thighs (like sciatica)
You may first notice symptoms after a muscle strain, so the condition is often mistaken for common backache.
Pain in your neck, shoulders, hips or thighs may follow. Some people also have pain, stiffness and swelling in their knees or ankles, or in the smaller joints of their hands and feet. For some people, especially children, the first signs may be in their hip or leg rather than their back.Other possible symptoms include:
• tenderness in your heel bone, making it uncomfortable for you to stand on a hard floor
• tenderness at the base of your pelvis (ischium), making sitting uncomfortable
• pain and swelling in a finger or toe – when the whole digit is swollen it’s known as dactylitis
• chest pain or a ‘strapped-in’ feeling if your spine is affected at chest level, which makes it difficult for you to take a deep breath
• an inflamed iris (uveitis or iritis) – see your doctor immediately if you suddenly develop pain or redness in your eyes
• tiredness caused by the activity of the condition, anemia or sometimes depression and frustration associated with the condition
• bowel problems known as inflammatory bowel disease (IBD) or colitisWho gets ankylosing spondylitis?
Ankylosing spondylitis can affect anyone, young or old, male or female, although it’s more common in young men. It’s most likely to start in your late teens and 20s.
Ankylosing spondylitis is linked to the genes we inherit. But if your parents have it it’s not definite that you’ll develop it. Ankylosing spondylitis affects 2-3 times as many men as women. The genes you inherit from your parents may make you more likely to develop AS, but the condition isn’t passed on directly. AS isn’t contagious so you can’t catch it from someone else.Most people with ankylosing spondylitis have a gene called HLA-B27, which can be detected by a blood test, but having this gene doesn’t mean you’ll get AS. Even in families where somebody has AS, a brother or sister may have the HLA-B27 gene and never get the condition.
How is ankylosing spondylitis diagnosed?
There’s no specific test for ankylosing spondylitis, so your doctor will base your diagnosis on your symptoms and how they developed, an examination, and blood tests, Χ-rays or scans. X-rays can show changes in your spine as the condition develops but aren’t always helpful in the early stages. Magnetic resonance imaging (MRI) scans may be useful when Χ-rays aren’t.Most back pain isn’t caused by ankylosing spondylitis. However, the symptoms of AS, especially in its early stages, are often very similar to the more common back problems, e.g. spinal disk herniation. Because of this, it can take some time before AS is diagnosed – it may even be misdiagnosed at first.
What tests are there?
A blood test can show inflammation in the body. You’ll probably have a C-reactive protein (CRP) or an erythrocyte sedimentation rate (ESR) test. Another blood test can confirm whether you have the HLA-B27 gene. Most people with ankylosing spondylitis test positive for HLA-B27, but so do some people without the condition. A positive test may point to AS but it won’t confirm the diagnosis.You may initially be asked to have an MRI if X-rays don’t show anything unusual. As the condition progresses, new bone develops between the vertebrae, which will be visible in X-ray images.
What treatments are there for ankylosing spondylitis?
There are many different treatments available, including exercises, tablets and injections. Your healthcare team can help you find suitable treatments, including:
• physiotherapy and regular exercise
• drugs
• surgery in more severe cases after a whileThese treatments aim to relieve your symptoms (e.g. pain and stiffness), keep your spine and other joints mobile and help you to live a normal life. Exercise, close attention to your posture and body weight are also important in reducing the impact of the condition to your quality of life.
Drugs
• Painkillers (analgesics) and non-steroidal anti-inflammatory drugs (NSAIDs) will relieve pain, which will help you to get a good night’s sleep. They can also ease stiffness, making it easier for you to exercise. You’ll probably need tablets during bad patches.
• Slow-release NSAIDs are effective over a longer period, so they may help with your night-time pain and morning stiffness. Pain-relieving tablets can sometimes irritate your stomach, but this should be less of a problem if you take them with food. However, if this happens, you should discuss it with your physician.
• Disease-modifying anti-inflammatory drugs (DMARDs) are designed to reduce damage to your joints rather than just ease your symptoms. They’re slow-acting so you won’t notice an immediate impact, but they’re very effective over a period of time. They’re more useful for symptoms in your arms and legs than in your spine. Some examples of DMARDs include leflunomide, sulfasalazine and methotrexate.
• Biological therapies, usually with anti-TNF factors, are given as an injection under your skin or intravenously. Biological therapies aren’t suitable for everyone and your doctor may ask you to have further tests, e.g. to rule out tuberculosis, before proceeding with the treatment.
• Steroids (cortisone) can be used as a short-term treatment for flare-ups. They’re usually given as an injection into a swollen joint, as a slow-release injection into your muscle or in the form of tablets. While these treatments can be very effective at improving the symptoms, you may develop side-effects if you use them for long periods, which you must discuss with your doctor.
Physical therapies
• Physiotherapy is a very important part of the treatment for ankylosing spondylitis. A physiotherapist can put together a program of exercises that increase your muscle strength, help you maintain mobility in your spine and other joints and help relieve the symptoms of inflammation. It’s especially important to exercise your back so that it doesn’t stiffen in a bent position.
• A physiotherapist may also be able to offer you hydrotherapy, which involves special exercises in a warm-water pool. Many people with AS find this therapy helpful.Surgery
Most people with ankylosing spondylitis don’t need surgery, though some may need a hip or knee replacement if their joints are badly affected. This can get rid of pain and improve mobility. Surgery to straighten a bent spine is very rare and isn’t usually recommended.- © 2007-2025 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.