- HYGEIA
- Vision & Mission
- Timeline
- Organizational structure
- Press Releases
- Social responsibility
- Awards and Distinctions
- Human Resources
- Scientific & Training activities
- Articles – Publications
- Our Facilities
- Magazines
- Healthcare Programs
- Doctors
- Services
- Medical Divisions & Services
- Imaging Divisions
- Departments
- Units
- Centers of Excellence
- Emergency – Outpatient
- Nursing Service
- Ambulances
- Patients
Spine Surgery
The philosophy of the 1st Neurosurgical Department in what concerns the management of spinal column diseases is focused to the individualized treatment of each and every patient by combining all the latest advances and technologies available in the field of spinal surgery. It is for this purpose that all treatments are delivered within the framework of the Spine Department, in collaboration with colleagues from other specialty domains such as orthopaedics surgeons, anaesthesiologists, rehabilitation physicians and the physical therapists. The 1st Neurosurgical Clinic offers surgical management of spinal degenerative diseases, spinal tumours (benign/malignant) and traumatic spine injuries. We also treat spinal cord pathologies: spinal cord tumors (benign and malignant) and spinal cord vascular lesions.
The following is an overview of the most common spinal conditions managed by the Neurosurgical Clinic (lumbar and cervical disc hernias, vertebral column and spinal cord tumours)
Intervertebral disc herniation is usually degenerative in origin. It is a process which affects both the disc itself and the vertebral bodies, the ligaments and the muscles supporting the spine. The disc consists of a soft core (nucleus pulposus) and a hard ring (annulus fibrosus), which surrounds the former. Along the course of a degenerative disease the outer ring undergoes a gradual loss of integrity resulting in the nucleus pulposus prolapse, which deteriorates over time, exerting pressure on the anatomical structures nearby and causing pain. In advanced stages part of the nucleus pulposus makes a large protrusion in the spinal canal producing the so-called (free- fragment) disc herniation. It is this situation that the patient experiences pain not only in the lower back (lumbago) but in the leg as well (sciatica). Even though low back pain may become extremely painful, it goes away in 90% of the cases without surgery. The therapeutic approaches include physical therapy,weight loss, epidural steroid injections (cortisone), nonsteroidal anti-inflammatory drugs and decreasing the level of physical activity. All the above approaches aim to decrease the inflammation in the lower back and the minimization of the nerve roots irritation. Traditionally 4 to 6 weeks of conservative treatment is recommended before suggesting surgery to the patient. Surgery is indicated if:
- The pain in the back or the leg restricts daily activities or has a negative effect on quality of life despite the medical treatment and the physical therapy
- There is a development of neurological symptoms, such as leg weakness and numbness
- There is loss of bladder / bowel sphincter control with resultant incontinence
If surgery is indicated, there is a number of procedures available to decompress the nerve roots affected. The one most commonly used is microdiscectomy.
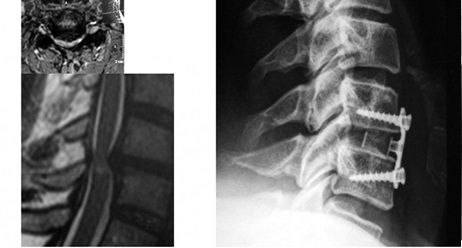
LUMBAR MICRODISCECTOMY
Lumbar microdiscectomy is carried out with the use of a surgical microscope and a microsurgical technique. Since microdiscectomy is performed under the surgical microscope, a relatively small skin incision is needed. A very small piece of bone is removed from the vertebral lamina. When the nerve under pressure is identified, the extent of the pressure exerted upon it by the herniated nucleus pulposus is defined with precision. Using a microsurgical technique, the herniated nucleus pulposus is removed. The surgery is completed with the suturing of each layer of the surgical wound. A few hours after the procedure the patient is mobilised and most of the times is released from hospital the following morning. The patient is advised to rest for 7- 10 days and is then allowed to gradually resume the daily activities.
Cervical disc microsurgical excision is a procedure performed in the upper part of the spine, between the 2nd cervical and the 1st thoracic vertebra, in order to relieve the pressure exerted upon one or more nerve roots or the spinal cord. When an intervertebral disc in the cervical spine is degenerated, it may prolapse (intervertebral disc hernia) and compress one or more nerve roots or the spinal cord (cervical myelopathy) causing pain to the neck, to the upper extremities and loss of sensation in the upper extremities (tingling – numbness). It may also affect the function of the lower extremities and the control of the bladder. Nerve root and / or spinal cord compression may also be the result of a vertebral deformity or of bone spurs (osteophytes – degenerative disease).
Surgical treatment indications
If conservative treatment for neck pain fails, surgery may be necessary. Indications for surgery are:
- The pain in the neck or the hand restricts daily activities or affects quality of life.
- There is a gradual development of neurological symptoms, such as upper extremities weakness and/or numbness.
- There are gait abnormalities and/ or loss of the bladder and bowel sphincter control.
- Failure of the medical treatment and physical therapy.
- Cervical myelopathy (spinal cord swelling –oedema- due to chronic spinal cord compression injury).
Cervical disc herniation
48-year-old patient with cervical disc herniation and focal spinal cord myelopathy (left). The patient underwent an anterior cervical microdiscectomy and instrumented fusion with a cage and an anterior plate (right).
If surgery is indicated, the neurosurgeon has a number of options to decompress the nerve roots involved. The most commonly performed surgery is the anterior cervical microdiscectomy. During the procedure the prolapsing intervertebral disc and any coexistent bone spurs (osteophytes) are removed decompressing the spinal cord and the cervical nerves. An implant (cage) is then placed (plastic polyetheretherketone – PEEK) with or without a supporting titanium plate in the anterior surface of the spine. In selected cases (young patients without significant degenerative lesions in other areas of the neck) a cervical disc prosthesis (Baguera) is implanted instead of a cage. The artificial disc has proven to be highly effective in maintaining range of motion in the operated level. However, no randomised control trial has confirmed yet the long-term benefits of the cervical disc prosthesis over the instrumented (cage) fusion technique.
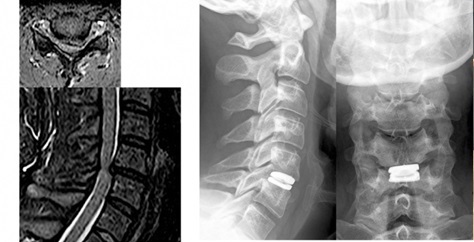
Cervical disc herniation
35-year-old patient with cervical disc herniation, which led to gradual muscle weakness of the left upper and lower extremities due to myelopathy (prolonged compression of the spinal cord because of spinal canal stenosis) (left) The patient underwent an anterior cervical microdiscectomy with artificial disc replacement (right).
Patients are mobilized out of bed the same evening of the surgery and they are usually discharged from the hospital within 24 hours. In surgeries involving more than one levels it may be considered necessary to extend hospitalization for 1-2 days. It is usually not necessary to apply a cervical orthosis after surgery.
The most common initial symptom is pain, which gets worse in bed, contrary to what happens with degenerative diseases. The pain may radiate to the spine, the hips, the legs or the arms and usually gets worse by time despite of the use of analgesics. Depending on the location and the type of the tumor other symptoms may develop as a result of the displacement or involvement of nerve structures, vertebrae and vessels; they include weakness or paralysis of an extremity or extremities, difficulties in walking, worsening or loss of the fine motor skills, reduction of sensitivity to pain, hot or cold stimuli and loss of bladder and/or bowel sphincter control.
Tumors are classified according to their anatomical location in the spine as follows:
- Extradural tumours (75%). The most common extradural tumours are secondary metastases. Metastases spread to the spine from a primary malignant tumour developed in another part of the body. Primary tumours (tumours growing from the bones of the spinal column itself) are less frequent. They can be either benign (osteoid osteomas, osteoblastomas, vertebral haemangiomas) or malignant (osteosarcomas, Ewing sarcomas, multiple myelomas).
- Intradural extramedullary tumours (20%). These tumours grow in the arachnoid membrane of the spinal cord (meningiomas), in the nerve roots that extend out of the spinal cord (neurinomas or neurofibromas), or along the filum terminale (ependymomas).
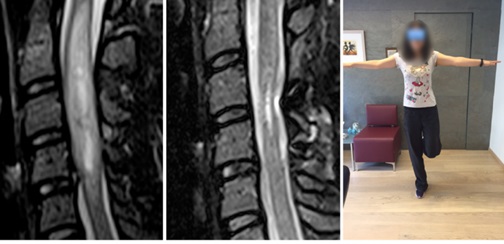
Cervical spinal cord ependymoma.
32-year-old patient with unstable gait, numbness and extremity weakness. The intramedullary tumor was totally removed with no further neurological impairment. Within a period of 6 months the patient was almost symptom – free and had resumed all her prior daily activities.
- Intramedullary tumours (5%). Most of the times they are either astrocytomas or ependymomas. Intramedullary metastases appear very rarely.
Magnetic Resonance Imaging is the imaging modality of choice for the diagnosis of spinal column tumors. Computer Tomography (CAT scan) is sometimes indicated to clarify the degree of the bony (vertebral body) erosion / invasion as well as for the planning of surgery. A bone scan helps in determining the extent of the spread of the metastatic disease to the bones.

Thoracic spine meningioma
54 year old patient with progressive lower extremities weakness and gait instability for about six months. She reported a torso and lower extremity sensory impairment and bladder dysfunction ten days prior to her admission in the hospital. The thoracic spine MRI scan disclosed an intradural extramedullary tumor. The tumor was totally resected through a posterior approach (laminectomies). Postoperatively the gait and the bladder function improved gradually. The patient had a mild numbness in the soles and the legs bilaterally postoperatively.
Ideally the goal of the treatment goal for the spinal column and spinal cord tumors would be the total removal and the restoration of the spinal stability protecting the functional integrity of the neural structures. In the decicion making for the best available treatment we consider the following parameters: the patient’s neurological presentation, age, general state of health, the type and localisation of the tumor and whether the tumour is primary or secondary (metastatic). The treatment choices include:
- Follow up with frequent imaging. Quite often tumors are randomly diagnosed before they cause symptoms while the patient is undergoing diagnostic evaluation for other reasons. Benign, small in size tumors, without significant compression or displacement of the neural structures or intramedullary tumors causing only mild symptoms and significant intraoperative risks, are managed with a regular follow up (conservative treatment). Conservative treatment is the treatment of choise in patients of advanced age and in all those patients with a significant risk of neural tissue irreparable damage in surgery or from radiation therapy.
- Surgical management. This is often the first step in the treatment of tumors, which may be removed with an acceptable risk of postoperative neurological compromise. The advancement of the microsurgical techniques has made possible the total resection of tumors which were thought to be inoperable untill recently. possible today to fully remove tumours which were regarded as inoperable up until recently. Usually the most benign tumors are totally resected. Total resection is not always feasible in metastatic or invasive intramedullary tumors. Actually the treatment of choise in the metastatic spinal tumors is radiation therapy and surgery is only indicated when a progressively worsening neurological deficit develops or spinal column instability is diagnosed.
- Radiation therapy. It may be delivered postoperatively to control the residual disease and avoide the recurrence. It is also indicated as a treatment of inoperable tumors. It is the treatment of choice (first line) for metastatic spinal tumors. Radiation therapy may also be applied for pain relief as a palliative treatment.
- Chemotherapy. Chemotherapy has not proven beneficial for most spinal column or spinal cord tumours. When indicated is always administered in combination with surgical treatment and/or radiotherapy.
- © 2007-2025 HYGEIA S.M.S.A.
- Personal Data Protection Policy
- COOKIES Policy
- Terms of Use
- Privacy Policy
- Credits
- Sitemap
- Made by minoanDesign
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.
Αποδοχή όλων Άρνηση όλων ΡυθμίσειςCookies ManagerΡυθμίσεις Cookies
Ο ιστότοπoς μας χρησιμοποιεί cookies για να καταστήσει την περιήγηση όσο το δυνατόν πιο λειτουργική και για να συγκεντρώνει στατιστικά στοιχεία σχετικά με τη χρήση της. Αν θέλετε να λάβετε περισσότερες πληροφορίες πατήστε Περισσότερα ή για να αρνηθείτε να παράσχετε τη συγκατάθεσή σας για τα cookies, πατήστε Άρνηση. Συνεχίζοντας την περιήγηση σε αυτόν τον ιστότοπο, αποδέχεστε τα cookies μας.




































